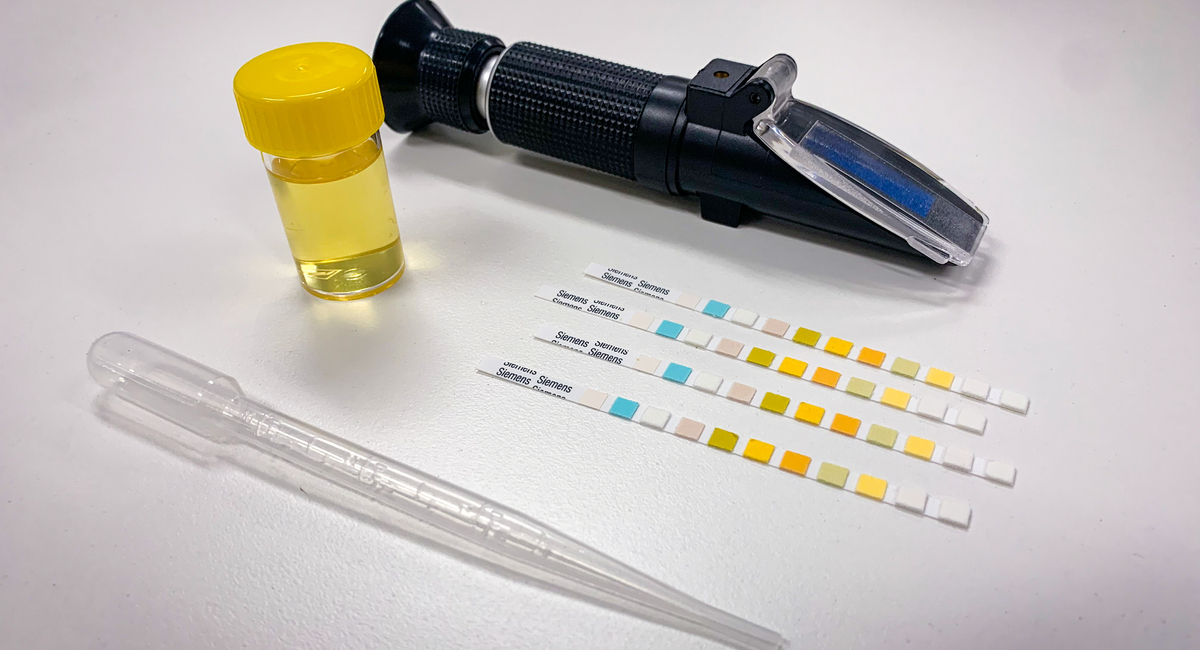
A common question we get asked at MX3 is how Salivary Osmolarity (SOSM) measurements made with the MX3 Hydration Testing System compare to Urine Specific Gravity (USG) in relation to dehydration. USG spot-checks are routinely used by many work sites and sports teams, but recent research reveals that this method can greatly over-estimate or underestimate the number of dehydrated individuals. This post will summarize some of the studies investigating USG and SOSM so you can better understand how these hydration biomarkers match up.
USG spot checks are highly variable and impacted by diet, activity and fluid intake
While USG has been widely adopted for hydration testing due to it being a reliable hydration indicator first thing in the morning, applying USG for spot-checks can be highly variable due to the influence of recent activity, diet and fluid intake on urine production1,2. In addition, first morning urine collection requires an individual obtain enough sleep and collect urine mid-stream. For these reasons, when USG is used for spot-checks hydration assessments the results can be inaccurate, lead to inappropriate actions relating to rehydration and impact safety and performance.
USG measures can also be subject to manipulation, whether intentionally or unintentionally, as workers or athletes need to collect and supply their samples. Given accurate hydration assessment with USG can only be achieved upon waking, assessment directly before, during or after a shift or training session, when it matters most, is not a valid approach.
Two recent studies have compared USG spot-checks and plasma osmolality measurements, that are used clinically to determine hydration status. In one study USG measurement greatly overestimated the proportion of athletes that were dehydrated prior to exercise, with 27% of athletes appearing dehydrated by USG but hydrated when looking at their plasma3. In another study approximately 65% of hydrated individuals appeared dehydrated by USG4. USG spot checks can additionally also overestimate hydration status5.
This variability can lead to many workers and athletes being unnecessarily excluded from work or training or conversely allowed to work or train when they are dehydrated. Based on these, and other studies, recent athletic guidelines do not recommend the use of USG spot-checks for hydration assessment6.
SOSM– An improved tool for spot-check hydration assessment
Salivary osmolarity (SOSM) is the concentration of particles, predominantly electrolytes, per liter of saliva. Multiple studies have shown that spot checks of SOSM provide an accurate assessment of changes in hydration status7-9. In a clinical context, SOSM spot checks have been demonstrated to be an effective tool for hydration assessment in the elderly10. USG was not an effective tool in this study.
Despite the convenience and non-invasiveness of measuring saliva, SOSM has been considered impractical for field testing of hydration due to the cost and lack of portability of laboratory osmometers. The MX3 Hydration Testing System overcomes these barriers, providing a simple, low-cost and rapid way of measuring SOSM.
There are a few limitations to SOSM that users should be aware of when using the MX3 HTS for field hydration assessment. Firstly, recent food and drink can contaminate saliva so it’s important to wait 5 minutes to allow SOSM to return to normal. It’s also important to use the correct sampling methodology to ensure enough saliva is produced and collected by the HTS. This involves generating a fresh saliva sample for collection, avoiding the sampling of bubbles and not immersing the sensor strip in saliva, but rather just sampling a small amount by tapping the sensor onto a wet tongue. We also understand that there is some biological variation in saliva, due to differences in composition produced by different salivary glands, therefore, the same individual may present readings fluctuating by +/-15% While this should be considered when interpreting measurements close to hydration assessment thresholds we find SOSM changes related to dehydration are substantial and so this variability does not prevent assessment of hydration status.
Conclusion
USG has been a widely adopted standard for hydration assessment for many years, although it has been widely used inappropriately. Recent studies have shown that reliance on USG spot-checks can greatly over- and underestimate the number of dehydrated athletes or workers. Using SOSM to monitor and track hydration status via the MX3 HTS provides an alternative, quick, convenient and accurate way to assess hydration status in athletes and workers to help them prepare, perform and recover from both work and training activities.
Find out more about the MX3 Hydration Testing System.
References
1. Cheuvront, S. N., Munoz, C. X. & Kenefick, R. W. The void in using urine concentration to assess population fluid intake adequacy or hydration status. Am J Clin Nutr 104, 553-556, doi:10.3945/ajcn.115.129858 (2016).
2. Cheuvront, S. N., Kenefick, R. W. & Zambraski, E. J. Spot Urine Concentrations Should Not be Used for Hydration Assessment: A Methodology Review. Int J Sport Nutr Exerc Metab 25, 293-297, doi:10.1123/ijsnem.2014-0138 (2015).
3. Hew-Butler, T. D., Eskin, C., Bickham, J., Rusnak, M. & VanderMeulen, M. Dehydration is how you define it: comparison of 318 blood and urine athlete spot checks. BMJ Open Sport Exerc Med 4, e000297, doi:10.1136/bmjsem-2017-000297 (2018).
4. Sommerfield, L. M. et al. Validity of urine specific gravity when compared to plasma osmolality as a measure of hydration status in male and female NCAA collegiate athletes. Journal of strength and conditioning research/National Strength & Conditioning Association 30, 2219 (2016).
5. Oppliger, R. A., Magnes, S. A., Popowski, L. A. & Gisolfi, C. V. Accuracy of urine specific gravity and osmolality as indicators of hydration status. Int J Sport Nutr Exerc Metab 15, 236-251, doi:10.1123/ijsnem.15.3.236 (2005).
6. McDermott, B. P. et al. National Athletic Trainers' Association Position Statement: Fluid Replacement for the Physically Active. J Athl Train 52, 877-895, doi:10.4085/1062-6050-52.9.02 (2017).
7. Walsh, N. P. et al. Saliva parameters as potential indices of hydration status during acute dehydration. Med Sci Sports Exerc 36, 1535-1542 (2004).
8. Smith, D. L., Shalmiyeva, I., Deblois, J. & Winke, M. Use of salivary osmolality to assess dehydration. Prehosp Emerg Care 16, 128-135, doi:10.3109/10903127.2011.614044 (2012).
9. Munoz, C. X. et al. Assessment of hydration biomarkers including salivary osmolality during passive and active dehydration. Eur J Clin Nutr 67, 1257-1263, doi:10.1038/ejcn.2013.195 (2013).
10. Fortes, M. B. et al. Is this elderly patient dehydrated? Diagnostic accuracy of hydration assessment using physical signs, urine, and saliva markers. Journal of the American Medical Directors Association 16, 221-228 (2015).